Tests for gestatonal diabetes at home
Diabetes in Pregnancy
Diabetes in Pregnancy or Gestational Diabetes also known as maternal diabetes or diabetes during pregnancy, is a type of diabetes that develops in some women during pregnancy.
Get insights into this condition, diagnostic tests, and management. We at Medilife offer you tests for pregnant females at your doorstep.

Gestational Diabetes: Overview
Pregnancy is a transformative time in a woman’s life, marked by numerous physiological changes. One of the most critical aspects of prenatal care is monitoring blood glucose levels, as this can impact both maternal and fetal health.
Gestational diabetes, also known as maternal diabetes or diabetes during pregnancy, is a type of diabetes that develops in some women during pregnancy. It occurs when the body cannot produce enough insulin to meet the increased needs of pregnancy, leading to elevated blood sugar levels.
Blood glucose testing during pregnancy is essential for screening and diagnosing.
What are the risk factors for gestational diabetes?
- Being overweight or obese before pregnancy.
- Having a family history of diabetes.
- Being over the age of 25
- Having had gestational diabetes in a previous pregnancy
- Polycystic ovary syndrome (PCOS)
Effects of high sugars on pregnancy?
- High blood sugar can affect both the mother and the baby. It may increase the risk of high birth weight, preterm birth, or complications during delivery.
- Babies born to mothers with gestational diabetes are at higher risk of developing obesity or type 2 diabetes later in life.
- Mothers are at a higher risk of developing type 2 diabetes after pregnancy.
Thus, glucose testing ensures that expectant mothers maintain normal blood sugar levels and take necessary precautions if abnormalities are detected
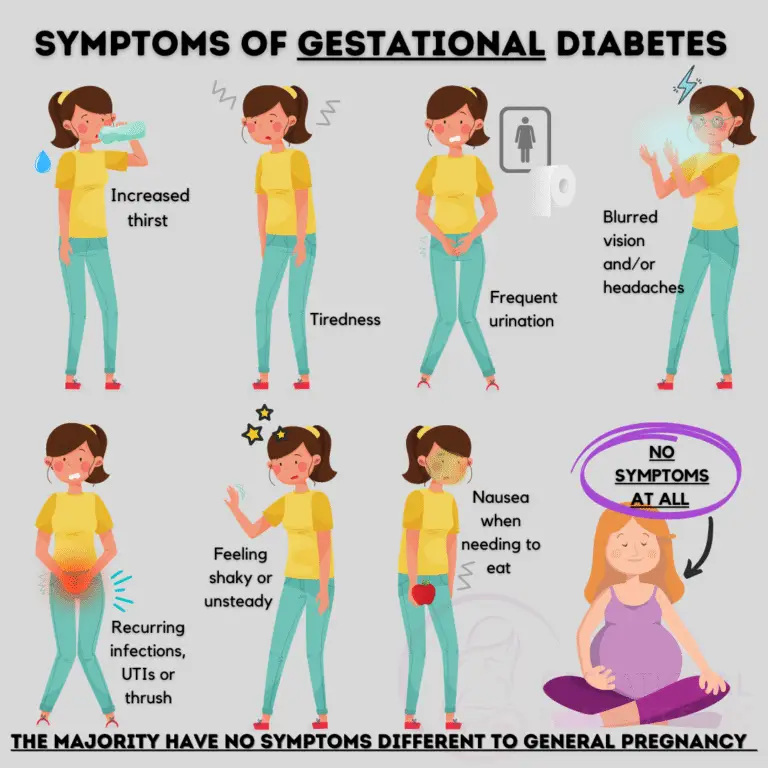
Most women with gestational diabetes do not experience noticeable symptoms/ symptoms are similar to those due to pregnancy.
- Increased thirst.
- Tiredness
- Frequent urination.
- Headaches/blurred vision
- Recurrent UTIs or thrush
- Nausea when needing to eat.
- feeling shaky or unsteady.
Types of glucose tests in pregnancy:
Glucose Screening Test for Pregnancy:
This is a routine test done between the 24th and 28th weeks of pregnancy. It is a preliminary test that helps determine whether a woman is at risk for gestational diabetes.
- During this test, a pregnant woman is given a sugary drink containing a specific amount of glucose (usually 50 grams). After one hour, a blood sample is drawn to measure blood sugar levels. This is often referred to as a random glucose test, as it does not require fasting beforehand.
- If the test results show that blood glucose levels are elevated, usually above 140 mg/dL, the doctor will recommend a more detailed test called the oral glucose tolerance test (OGTT).
Prenatal Glucose Tolerance Test / OGTT
The oral glucose tolerance test (OGTT) is the follow-up test for women who have elevated results in the glucose screening test. This test is more comprehensive and requires fasting for at least 8 hours beforehand.
- A fasting blood sample is taken to measure baseline glucose levels.
- The pregnant woman drinks a solution containing a higher dose of glucose (usually 100 grams).
- Blood samples are drawn at intervals, typically at 1, 2, and 3 hours after consuming the glucose solution.
The OGTT measures how the body processes glucose over time. If two or more of the blood samples show elevated blood sugar levels, the woman is diagnosed with gestational diabetes.
Random Glucose Testing:
In some cases, random glucose testing may be performed at various points during pregnancy, especially if a woman has risk factors for gestational diabetes, such as obesity, a history of GDM in a previous pregnancy, or a family history of diabetes.
- This test measures blood sugar levels at any given time, without the need for fasting. Elevated random glucose levels may warrant further investigation with more detailed tests like the OGTT.
Diabetes Testing – Fasting:
- In addition to the glucose screening and tolerance tests, some healthcare providers may opt for a fasting blood glucose test as part of prenatal care. This test involves fasting for 8 to 12 hours and then measuring the blood sugar level.
- A normal fasting blood glucose level is below 100 mg/dL, while levels between 100 mg/dL and 125 mg/dL indicate prediabetes, and levels above 126 mg/dL indicate diabetes.
Management of Diabetes in Pregnancy:
If a woman is diagnosed with gestational diabetes, managing blood sugar levels becomes a critical part of prenatal care. Effective management reduces the risk of complications during pregnancy and childbirth.
Dietary Changes: The first line of treatment for gestational diabetes typically involves dietary changes with a balanced diet with controlled portions of carbohydrates to maintain stable blood sugar levels. Foods that have a low glycemic index, such as whole grains, vegetables, and lean proteins, are emphasized.
Exercise: Regular physical activity helps the body use insulin more effectively, which can lower blood glucose levels.
Walking, swimming, or prenatal yoga are often recommended for pregnant women with gestational diabetes.
Blood Sugar Testing at Home: Women diagnosed with gestational diabetes are often instructed to monitor their blood sugar levels regularly using a blood glucose test at home.
This involves pricking the finger with a small lancet, placing a drop of blood on a test strip, and using a glucose meter to read the blood sugar level.
Medication and Insulin: In some cases, lifestyle changes alone may not be enough to control blood sugar levels, and medication or insulin injections may be necessary.
maternal diabetes! tests for diabetes in pregnancy! blood test in pregnancy!
Common inquiries regarding diabetes in pregnancy
Gestational diabetes is a type of diabetes that develops during pregnancy when the body can’t produce enough insulin to regulate blood sugar levels.
Hormonal changes during pregnancy can make it harder for insulin to control blood sugar levels. If the pancreas cannot keep up with the increased demand for insulin, blood sugar levels rise, leading to gestational diabetes.
Women who are overweight, over the age of 25, have a family history of diabetes, or have had gestational diabetes in a previous pregnancy are at higher risk.
Other risk factors include certain ethnicities, like African American, Hispanic, or Asian.
Gestational diabetes is typically diagnosed between 24 and 28 weeks of pregnancy through a glucose tolerance test, which measures how well your body handles sugar.
Often, there are no noticeable symptoms. Some women may feel more thirsty or tired than usual, but these can also be common in pregnancy. That’s why screening is so important. The symptoms may include:
- Increased thirst.
- Tiredness
- Frequent urination.
- Headaches/blurred vision
- Recurrent UTIs or thrush
- Nausea when needing to eat.
- feeling shaky or unsteady.
Yes, if untreated, it can lead to complications like a larger baby (macrosomia), premature birth, or breathing problems at birth. It can also increase the risk of the baby developing diabetes or obesity later in life.
As soon as pregnancy is confirmed:
- Complete blood count
- Blood grouping and RH typing.
- HIV, HBsAg, VDRL
- Thyroid function tests (TSH, T3, T4)
- Fasting blood sugar or HBA1C
- Urine routine and culture.
- Vitamin D and B12 levels.
- MMR IgG antibodies.
In addition to tests done as soon as the pregnancy is confirmed, the following tests or diagnostic procedures have to be done:
- Dating ultrasound at 6-9 weeks to confirm gestational sac, heartbeat, and pregnancy.
- Nuchal translucency (NT) scan: 11-13 weeks, to detect chromosomal anomalies.
- Double marker test: blood test for Down syndrome screening.
- Anomaly scan at 18-22 weeks: to check fetal growth and organ formation.
- Triple or Quadraple test: for downs syndrome
- Blood Sugar Test: OGTT at 24-28 weeks to rule out maternal diabetes.
- Urine routine and culture.
- CBC—for anemia
- Iron, Vitamin D and B12 levels
Gestational diabetes can increase the chance of having a larger baby, which may lead to complications during delivery, including the need for a caesarean section. Your doctor will monitor your condition and help guide the safest delivery plan.
In most cases, blood sugar levels return to normal after delivery. However, having gestational diabetes increases your risk of developing type 2 diabetes in the future, so it’s important to maintain a healthy lifestyle after pregnancy.
